Akron Children’s Hospital Transport Quality Assurance Management Plan

The purpose of the Quality Assurance and Performance Improvement Plan (QAPI) for Akron Children’s Hospital transport service line is to provide direction and oversight for improving clinical and process performance with the goal of creating a safe environment and improving health care quality and patient outcomes. The plan describes key performance improvement activities and demonstrates the connection with the Akron Children’s Hospital quality structure. Akron Children’s Hospital Transport service line is aligned with our organization which subscribes to the Institute of Medicine’s six aims for health care:
- -Safe
- -Patient Centered
- -Effective
- -Efficient
- -Timely
- -Equitable
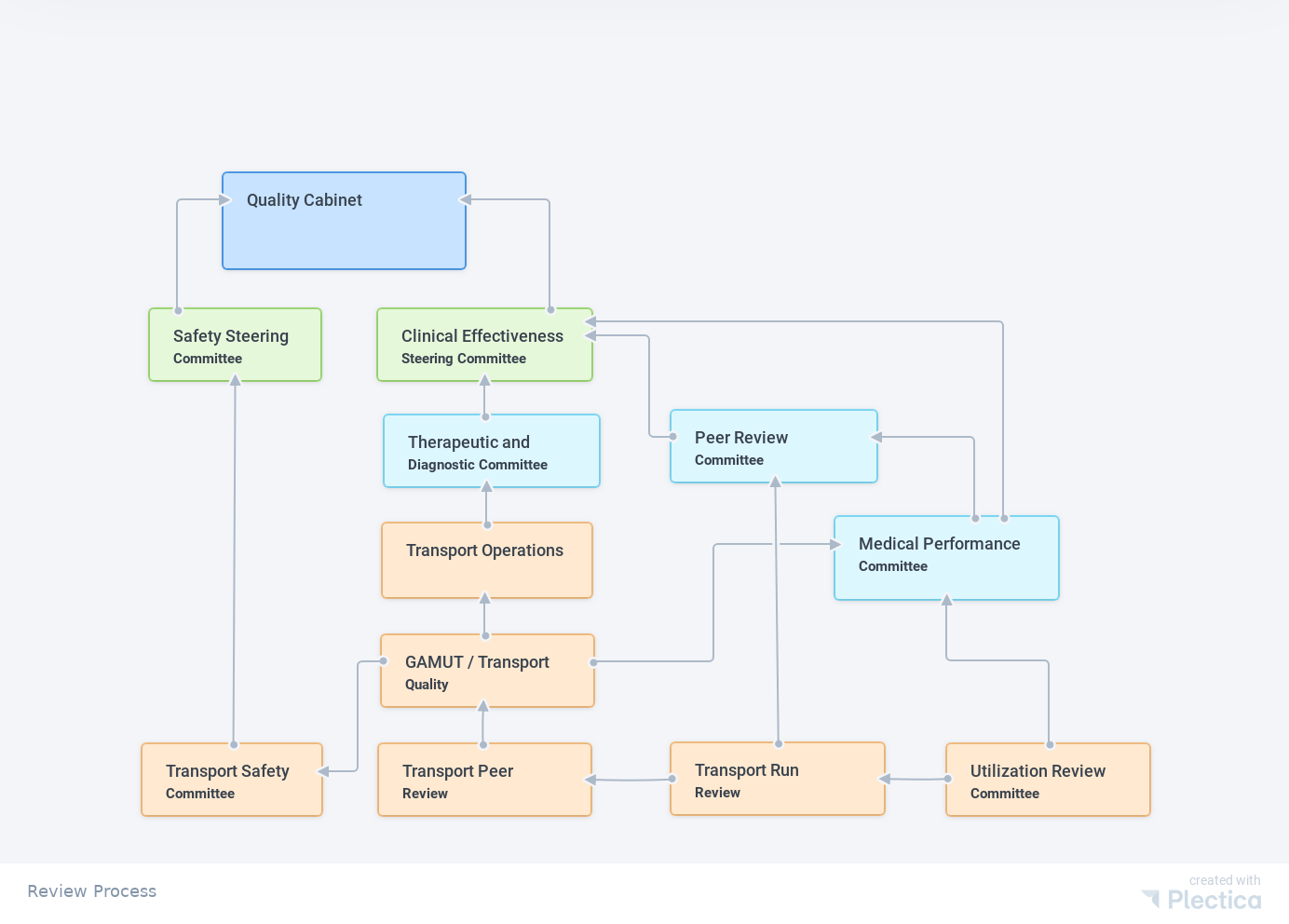
The transport quality committees are integrated into the organization’s quality structure formally through quality steering sub- committees (represented by blue boxes), which report to the organization’s Quality Steering Committees (Green Boxes) and ultimately to the Quality Cabinet. The orange boxes represent the transport department quality committees.
Transport quality review process
The organization’s Quality Cabinet is its quality governance committee. The Cabinet is composed of clinical and operational leaders from each of the quality steering committees as well as key members of the executive leadership team, including the Chief Quality Officer, Chief Medical Officer, Chief Nursing Officer, Chief Information Officer, Chief Nursing Information Officer and Chief Research Officer.
Quality improvement work germane to a department providing inter-facility air and ground transport is connected to the Quality Assurance Program Structure through:
Nursing representation on the Nursing Shared Governance Quality Council
Employee safety events are reported and improvement work connected to the Safety Steering Committee.
Patient quality outcomes as tracked through the GAMUT database and participation in the GAMUT collaborative report through Medical Performance Improvement Committee (A subcommittee of the Medical Staff Executive Committee).
Process outcomes are reported to the Therapeutic and Diagnostic Subcommittee of the Clinical Effectiveness Steering Committee
There is a bi-directional flow of quality information to improve patient, process and financial outcomes through:
- Information from the Peer Review Process (medical and transport) are used to identify and resolve systems issues. Dissemination of the identified opportunity to improve and the improvement plan are communicated through Transport Operations, as well as operational based meetings such as Transport Leadership, Unit Based Counsel and staff meetings.
- Identification and resolution of patient, employee and equipment safety issues and latent threats on air or ground transports through the Transport Quality Assurance and Safety Committees.
- Patient quality outcomes as tracked through the GAMUT database and participation in the GAMUT are shared with leadership and staff through Transport Staff Meetings.

Goals of the Quality Assurance Managment Plan
- Ensure accountability for quality with links to our organization’s strategic plan.
- Develop and sustain an infrastructure that significantly enhances the ability to continuously improve.
- Implement and optimize technologies and innovation to improve clinical and process outcomes.
- Ensure that quality improvements are developed and implemented consistent with evidence-based practice literature.
- Identify known, suspected or potential opportunities for improvement related to quality.
- Maintain and strengthen the quality assurance program to support the prevention and reduction of healthcare errors and hospital acquired conditions, and staff injuries by creating an environment conducive to identifying and managing actual and potential risks to safety.
- Establish priorities for the investigation and potential corrective actions/resolutions of concerns and issues by focusing on those with the greatest potential impact on quality.
- Maintain an ongoing, comprehensive and objective mechanism to measure, assess and improve the quality of patient care and through data collection and analysis.
- Set internal goals that align with national standards, benchmarks and trends, as well as best practice and evidence when available.
- To improve the documentation of and response to pain scores on transport.
- To meet or exceed CAMTS benchmark for:
- 1st time intubation success rate
- Ventilator use on transport
- Neonatal hypothermia
- Capnography use on transport
- Achieve 100% adherence to reporting serious safety, employee safety and hospital acquired conditions occurring during transport through the safety management reporting system.
- Reduce the number of days away return to work (DART) attributed to crew injury on transport
- Achieve an out the door time of 15 minutes from time of dispatch for air and ground transports.
- Report outcomes quarterly and as a year-end summary.
- Conduct utilization review of appropriateness of the mode of transport and team configuration
- Randomly review one chart per month from each mode of transport for:
- Appropriateness of transport mode
- Triggers include:
- Released from the emergency department following transport
- Transported without an IV
- Change in mode of transport prior to the team returning to definitive care.
- Triggers include:
- Appropriateness of team configuration
- Triggers include:
- Appropriateness of transport mode
- Randomly review one chart per month from each mode of transport for:
- Critical care dispatched while the ALS team is at the referral and has assumed care.